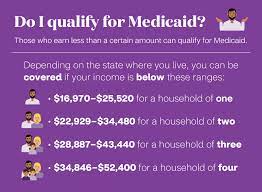
Medicaid, a collaborative initiative between the Federal government and states, plays a crucial role in ensuring healthcare access for individuals with low incomes, regardless of disability status. As a joint program receiving partial funding from the Federal government and administered by individual states, Medicaid tailors its eligibility criteria to meet unique needs. One significant transition in Medicaid eligibility occurs at age 18, marking a pivotal moment for individuals seeking healthcare coverage. Let’s delve into the details of Medicaid age eligibility and the implications of turning 18.
Medicaid Age Eligibility: A Guide to the Transition at Eighteen
Medicaid: A Lifeline for Low-Income Individuals
Medicaid stands as a vital program, bridging the gap in healthcare access for those with low incomes, irrespective of disability status. This collaborative effort between the Federal government and states allows for a flexible approach, with individual states tailoring their programs to address the specific needs of their populations.
Age 18 Transition: A Significant Milestone
Upon reaching the age of 18, individuals experience a notable shift in Medicaid eligibility. Termed as a “family of one,” parental income is no longer a determining factor for eligibility. This adjustment opens doors for many young adults who may have been ineligible due to their parents’ income levels.
Transitioning to Adult Medicaid
States that expanded Medicaid under the Affordable Care Act (ACA) provide coverage starting at age 19. This transition ensures a smooth shift from programs like Medicaid for children or the Children’s Health Insurance Program (CHIP) to adult Medicaid. The application process for Medicaid can be initiated through the HealthCare.Gov webpage, offering a user-friendly platform for individuals to explore their eligibility and apply for coverage.
Special Provisions for Former Foster Youth
Former foster youth benefit from specific provisions, with Medicaid coverage extending until age 26 for those exiting foster care at 18. This extension applies to individuals who were on Medicaid while in foster care or are ineligible for other Medicaid coverage. Notably, no income is counted towards eligibility in this group, providing flexibility even in the presence of alternative coverage options offered through employers.
Considerations for Adopted or Placed Individuals
Conversely, individuals adopted or placed in guardianship at age 18 are not eligible for Medicaid under the former foster care coverage group. This distinction underscores the nuanced considerations within Medicaid eligibility criteria.
Conclusion: Navigating Healthcare Transitions
Understanding the Medicaid age eligibility transitions, especially at the crucial age of 18, is essential for individuals seeking healthcare coverage. The flexibility and provisions offered by Medicaid, coupled with state-specific variations, contribute to a comprehensive approach to healthcare access. As individuals navigate these transitions, the goal remains to ensure that healthcare remains accessible, inclusive, and responsive to the diverse needs of the population.